New Case Study:
"High-Volume Emergency Department Boosts Efficiency by Adding Scribes"
A busy Emergency Department decided in early 2023 to explore solutions to address labor shortages and rising costs. Partnering with ScribeAmerica, they initiated 1:1 scribe coverage for all providers in the department.
Read more
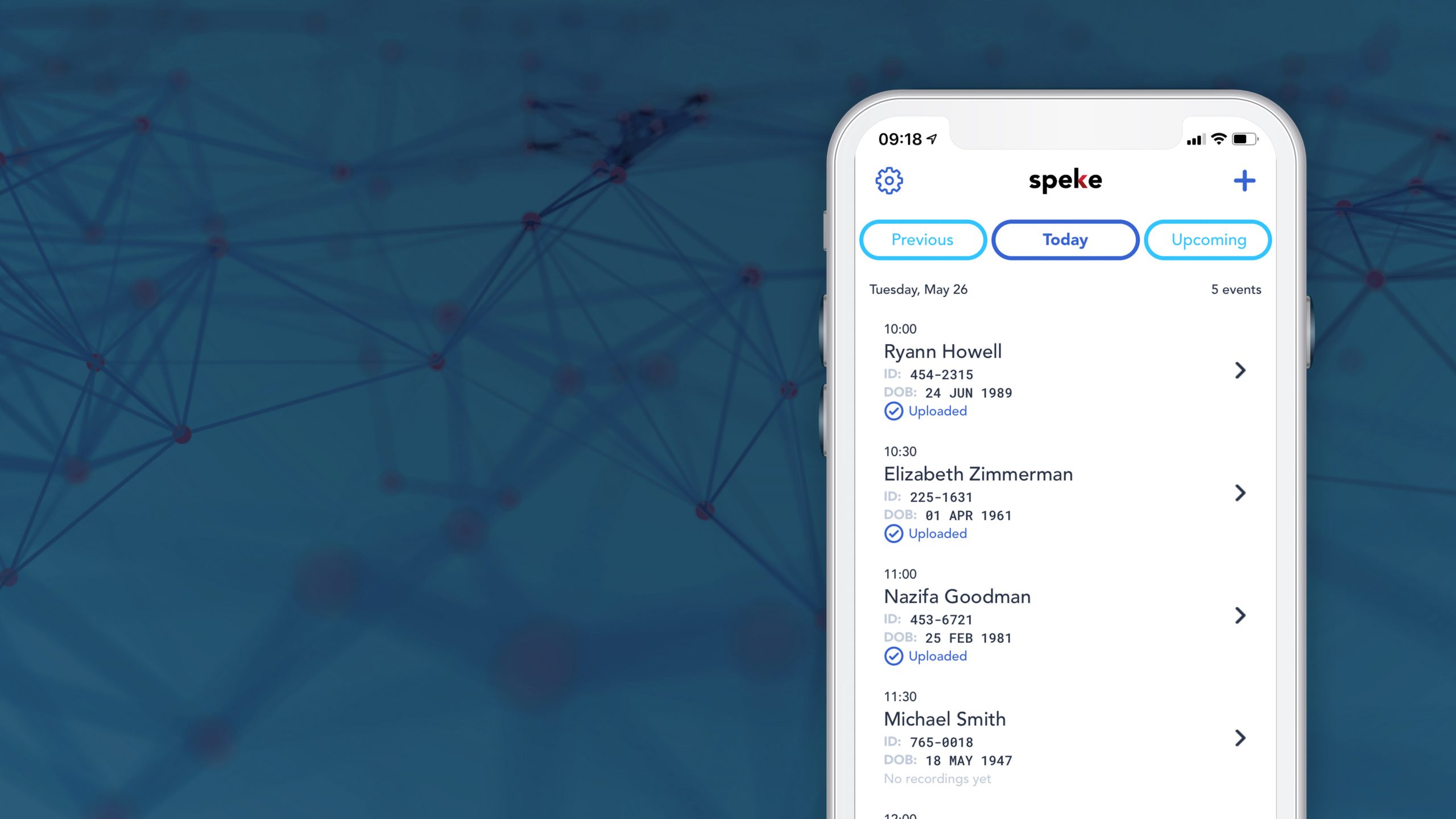
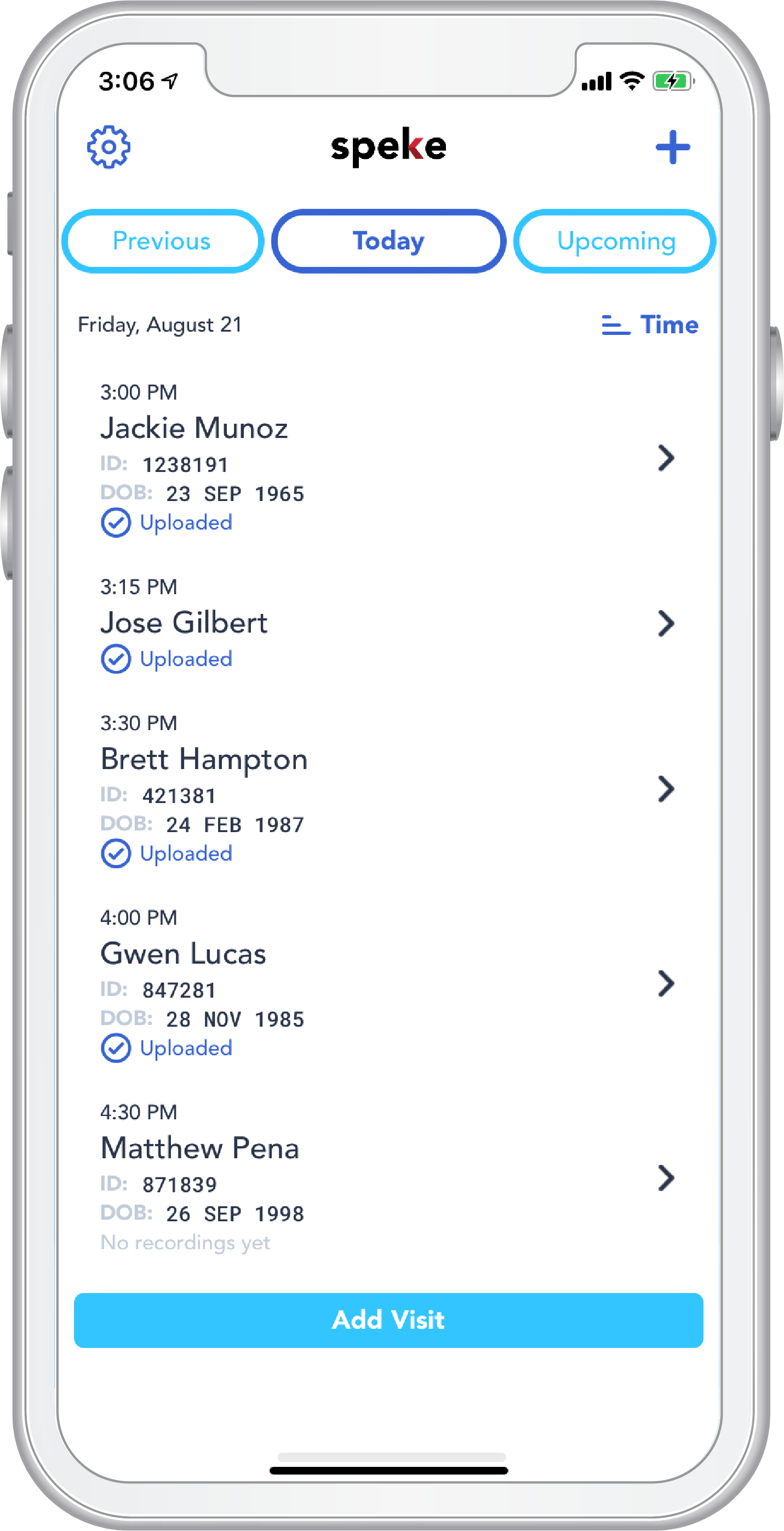
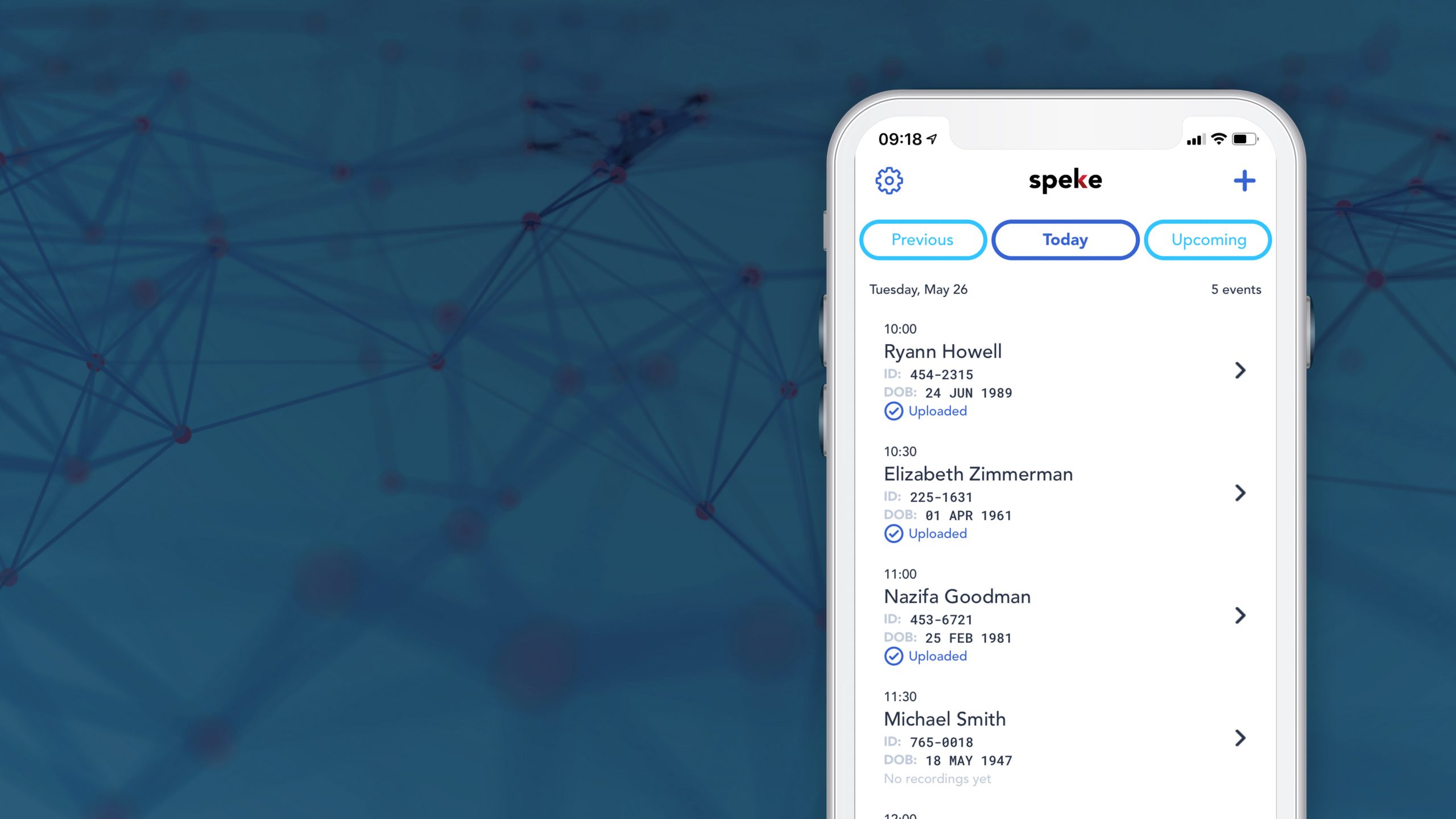
Speke, the first true ambient documentation assistant.
Integrating ambient technology so providers can practice medicine and focus on the patient again. Anywhere, with anyone.
LEARN MORE

Doctors Save Lives.
Scribes Save Doctors.
With scribes, providers can spend less time behind a computer and more time focused on delivering quality patient care.
LEARN MORE

Join the ScribeAmerica Team
ScribeAmerica is hiring! Jumpstart your career in healthcare with in-person and remote positions across the nation.
APPLY NOW

TeleScribes: Tailored Virtual Solutions from ScribeAmerica
No matter where or when you provide care for patients, TeleScribes transform your practice by delivering cutting-edge, engaged, documentation support.
Learn More
Delivering a full training and management medical scribe program, unparalleled in quality to any other in the industry.
Transform your practice with our state-of-the-art, engaged and custom remote support for patient-centered care.
Our seamless ambient AI scribe allows providers to shift away from the computer and back to the bedside.
Engage the unique populations you serve with a robust solution designed to assess social determinants of health.
Our skilled navigators go the extra mile by establishing critical touch points with patients and identifying barriers to care.
Offering services in multiple specialties, veterinary care teams will see reduced burden, decreased overtime and improved satisfaction.
KLAS Spotlight: Speke
The KLAS Emerging Technology Spotlight report examines customer experience and overall satisfaction using Speke, ScribeAmerica’s Ambient AI Scribe. Customers gave Speke high performance grades in all categories, and 100% said they would buy again. Additionally, respondents said Speke helped decrease provider burnout and increased capacity and available time with patients.
20 years ago we set the standard for scribes. Today, we’re redefining it.
We’ve often heard our scribes referred to as “Super Scribes.” Working in tandem with providers to deliver outstanding care, our medical scribes go beyond providing efficient documentation. From supporting pre-visit prep, to patient flow management, to care coordination and other non-clinical tasks, our scribes go the extra mile to act as productivity partners for your care team.
As burnout reaches epidemic proportions, these SuperScribes empower care teams to work top-of-license, joining providers with a background of exceptional training from the nation’s leader in scribe management.
Learn More
Scribes are the Next Generation of Leaders
Unlock the future leader in you. Start your journey with ScribeAmerica today!
Apply Today
Provider Spotlight: Dr. Fitzgerald, Emergency Medicine
“We have a choice between patient care or computer care. The scribes take the computer care so we can focus on the patients, which is what we’re all here for.” Hear Dr. Fitzgerald’s experience working with Emergency Scribes and how it helped to optimize the Hilo Medical Center ED.

The first true ambient AI scribe.
Integrating ambient technology so providers can practice medicine and focus on the patient again. Anywhere, with anyone.
Speke teams medical scribes with AI to create a reliable documentation assistant that lets you spend more time with your patients, not a computer. With scribes “in the loop,” your notes are completed accurately, efficiently and on time.
Read More
Latest News
The latest articles on ScribeAmerica, medical scribes and the latest in industry news.
September 5, 2023 – Medical Economics
What to look for in an AI scribe tool
Artificial Intelligence,
Burnout,
Innovation,
Machine Learning,
SA in the News
READ MORE
July 27, 2023 – Yahoo Finance
AWS this week unveiled a generative AI scribe for docs. The competition is fierce.
Artificial Intelligence,
SA in the News
READ MORE
July 13, 2023 – Urology Times
Is a medical scribe right for your practice?
Burnout,
Medical Scribes,
Optimize Documentation,
Provider Efficiency,
SA in the News
READ MORE
July 5, 2023 – Medical Economics
Scribes can provide numerous benefits to medical practices
Medical Scribes,
SA in the News
READ MORE
May 24, 2023 – Becker’s Healthcare
How physicians can help mitigate healthcare’s ‘recipe for disaster’
Burnout,
Medical Scribes,
SA in the News
READ MORE
October 31, 2022 – WKYC
Being a Medical Scribe May Help Northeast Ohio Students Write Their Health Care Future
Medical Scribes,
Provider Efficiency,
SA in the News
READ MORE
June 17, 2022 – JHMHP
Pairing a medical scribe with a hospitalist physician improved clinician satisfaction, increased productivity and provided a return on investment
Medical Scribes,
Patient Experience,
Provider Efficiency,
Provider Satisfaction,
SA in the News
READ MORE
May 17, 2022 – AMA
Burnout benchmark: 28% unhappy with current health care job
Burnout
READ MORE
April 19, 2022 – EHR Intelligence
Clinician Burnout, EHR Satisfaction Linked to Likelihood to Leave Org
Burnout,
Optimize Documentation
READ MORE
March 30, 2022 – AMA
Doctors hit hardest by pandemic at higher risk of burnout
Burnout
READ MORE
Our Record of Success
ScribeAmerica has earned profiles in numerous national news publications for our leadership and growth. From Inc 500/5000 recognition to Modern Healthcare, ScribeAmerica has received coverage in notable media outlets for delivering transformative results through a range of innovative Scribe Programs and care coordination solutions.